Be yourself; Everyone else is already taken.
— Oscar Wilde.
This is the first post on my new blog. I’m just getting this new blog going, so stay tuned for more. Subscribe below to get notified when I post new updates.
Be yourself; Everyone else is already taken.
— Oscar Wilde.
This is the first post on my new blog. I’m just getting this new blog going, so stay tuned for more. Subscribe below to get notified when I post new updates.
Use of monoclonal antibodies has expanded into the field of asthma with an FDA approved drug Benralizumab, a somewhat add-on asthma treatment for those who suffer specifically from eosinophilic asthma. The severity of this particular form of asthma is traced to an excess of white blood cells in an individual that increases inflammatory responses in the body, in this case the chronic inflammation is seen in the lungs and the tissue of that individual’s respiratory system. After offering a brief introduction into the world of monoclonal antibodies, it will become clear how perfect Benralizumab is for the job of fighting the overactive immune response. After all, it’s what they were made for.
I’m not even an artist, but I think understanding monoclonal antibodies is somewhat like understanding someone mixing paints colors to make the perfect picture. Say you want a beautiful pink color to paint a pig, the focal point of your drawing, but you only have red and white on your palette. Although without the added pressure of one’s life depending on it, this scenario is at its core similar to when the human body needs a certain antibody to fight off an antigen, and is looking at its palette containing B cells and Myeloma cells. Just as the red brings the dark heart of the color, B cells offer the capacity to make antibodies. Just as the white color brings the lightness to the color, myeloma cells bring plasma cells with the capacity to grow indefinitely, and are specifically susceptible to a drug known as aminopterin. Just like mixing paints, the making of monoclonal antibodies involves mixing together these qualities of B cells and myeloma cells to make a new cell with its own unique capacities. This “pink” is a hybridoma cell.

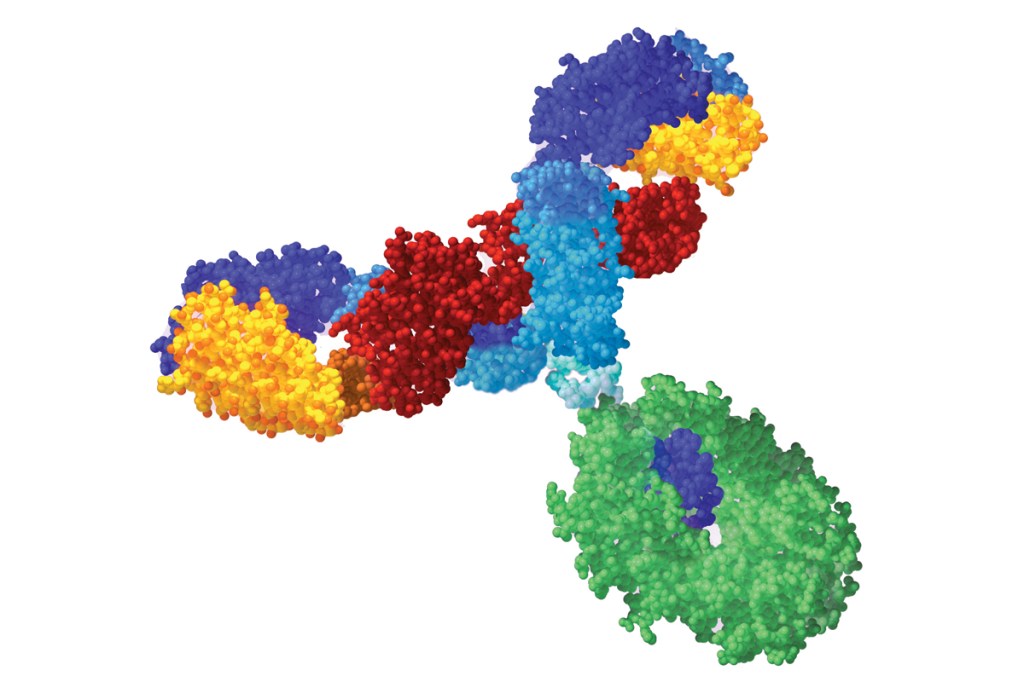
As no color mix is perfect, there’s usually a part of the paint mix that’s a little lighter or darker than another part, one of these fitting perfectly for your painting vision of the pig you set out to craft. This is similar to the production of hybridoma cells. As these fusion cells are made, there is one that fits perfectly with the antigen being targeted. It’s this hybridoma cell that will replicate and produce antibodies, just as it is that specific shade of pink you will select with your brush and spread on your canvas. The antibodies, being identical to one another, are able to fight off the particular antigen with maximum efficiency.
In the case of Benralizumab, the monoclonal antibody used for fighting eosinophilic asthma, specifically fights the excess production of eosinophil cells in the body that happen in response to an asthma trigger, causing severe inflammatory response of the airways and respiratory routes, leading to asthma symptoms. When these antibodies bind to the excess eosinophils they then can signal to the body’s immune system that these cells must be removed. The most extreme side effects of this drug are allergic hypersensitivity reactions, even days after an individual is injected with the drug. The most common side effects, however, consist of a sore throat and headache. Pregnancy and parasitic/helminth infections serve as preexisting conditions that increase dangers of using Benralizumab. It is also key to NOT stop taking other asthma medicine.
EXTRA CREDIT
As a history minor, I am passionate about the importance of fully understanding a situation by looking to the past. In other words, placing things in historical context. As the world of science continues to do everything in their power to move us forward, I will take us back about 100 years, to another period in history in which a virus was taking over the normalcy of America. The Polio epidemic, somewhat similar to the COVID-19 presence in America, had a strong center presence in New York. This epidemic took the lives of around 6,000 individuals, paralyzing those it did not kill. Also similar to today’s handling of COVID-19, this summertime epidemic brought a temporary end to things like pool time and gatherings.
Scientists reflect on this outbreak as an example of the importance of vaccination, as this disease went from one of the most feared diseases in the nation to eradicated since 1979. Traveling to other countries, where there is NOT herd immunity, increases the risk of obtaining this disease, as the US vaccination success has prevented the possibility of individuals being hosts of the disease.
The American people have been told to wash their hands, to try and scrounge up some purell, and try their best to avoid contact with any individual or object that might be a COVID-19 carrier. Beyond the (hopefully) closed doors of the quarantined American public are the front line fighters, the scientists looking to not hide from, but understand the COVID-19 virus. This blog will focus specifically on the developments made to fight corona related to antibody testing. The primary objective in testing was diagnostic, attempting to discover a method of sorting out who did and who did not have this disease. Very quickly, nose swabs began entering the canals of individuals. These swabs purpose is strictly to detect viral RNA proteins in the throats and noses of the symptom-presenting individual, specifically to determine the current presence of COVID-19 in an individual. With the progression of the disease, the testing objectives have broadened, focusing more largely on an individual’s whole immune system rather than simply the presence of the virus. At the start of the month, the FDA has thankfully approved a blood test that looks at an individual’s antibodies, seeing if they are equipped with the antibodies necessary to fight off the virus. Known as a serology-based test, these blood tests offer a look into the antibody responses of individuals to see the extent to which their immune system has interacted with the specific COVID-19 viral pathogen.
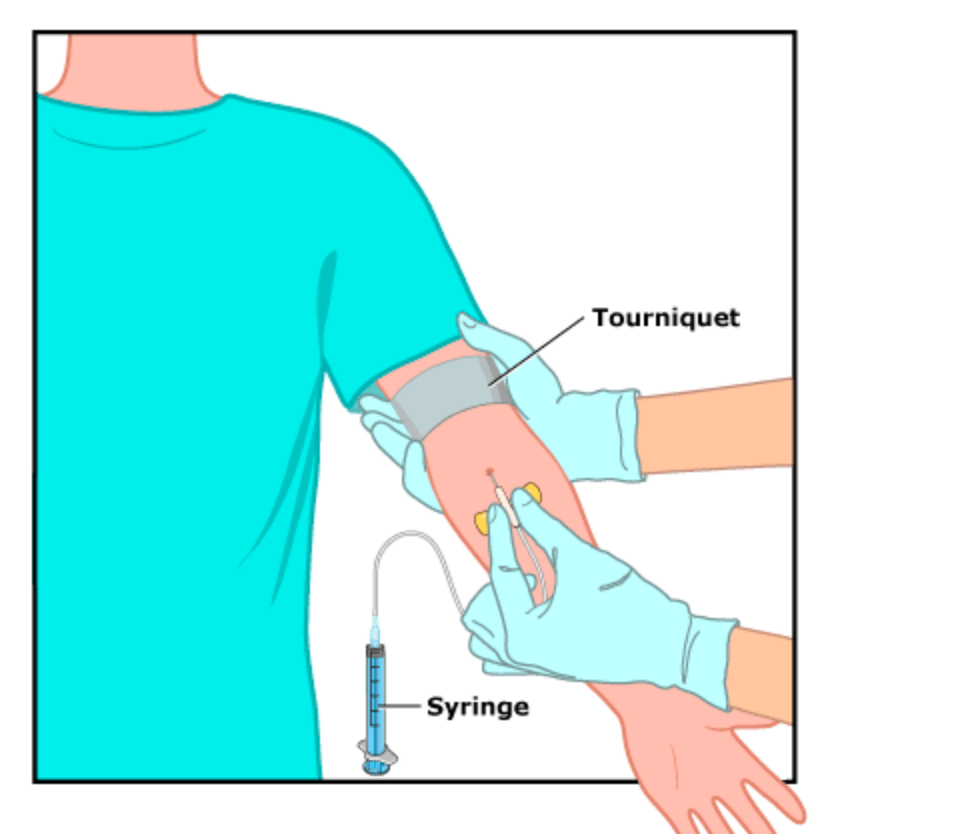
To help communicate the significance of this development, I’ll offer a little explanation into my understanding of antibodies, and why their presence is key to understanding COVID-19. The serology test measures the levels of antibodies in your blood that your body has made in response to a specific pathogen or invader. These antibodies survive long after the presence of that virus has gone, existing as a sort of preparedness to go back to battle in case your body comes across that pathogen again. Because of this, they are able to be detected in the blood. The first type of antibody produced by one’s immune system is known as IgM, which is produced by B cells when they are first exposed to a new pathogen or virus. B cells undergo a process known as class-switching in which the B cells are genetically modified and told by cytokines to produce better-fitting antibodies to the specific antigen being produced. IgG is this more effective antibody, that is able to be produced quickly after class switching in a B cell occurs. The B cells then produce clones then are capable of producing IgG, the more effective antibody. The IgG not only helps fight the pathogen more effectively, but their significance also comes into play when the body is introduced to that same pathogen again, meaning that the B cell clones are prepared to make only the most effective IgG antibodies. You can have both IgG and IgM in your blood as your body is encountering the initial pathogen and starting to make memory cells simultaneously. As the IgG levels increase, long term protection against that particular antigen is secured.
The presence of these antibodies in the blood can indicate very important things regarding COVID-19. If the blood test levels positively indicate the presence of IgG, this can indicate that the individual has encountered the COVID-19 virus before, whether or not that person even experienced symptoms the first time around. Also, the presence of IgG antibodies in the blood communicates that the individual will be able to effectively rid the body of the pathogen if meeting it again, meaning that they will not be able to transmit that virus to others. For COVID-19, understanding antibodies is especially important as the community looks to understand when it can return to normal societal operations. If a person’s blood tests indicate that they have the proper antibodies that make them immune to a re-infection, then the transition back into public will be safer, ensuring that that individual can not get or transmit the virus again.
EXTRA CREDIT:
To take our mind off one disease that has taken center stage in the recent months, what better than to turn our attention to a different one? A current disease outbreak mentioned by the CDC is the food borne illness, listeria. On March 9th and April 7th, two companies recalled their enoki mushroom production due to their relation to an outbreak in Listeria infections in consumers. Luckily, there have been no additional cases since March 27th! I have enjoyed researching this disease rather than COVID-19, because it has shown me a very small scale example of effective institutional action to prevent the spread of a disease. Although there were four deaths associated with this listeria outbreak, the recalls by the FDA were effective in keeping the food borne pathogen from being mass produced and given to the population.
In researching the impact of T cell therapy taking place in medicine around the world, my attitude on understanding effector cell activation has shifted dramatically. Each detail, while tedious to conceptualize while learning the material at home, is a piece of knowledge that brings the scientific community one step closer to providing a cure for cancer. In this blog, I will be sharing some things I’ve learned about the developing research regarding T cell therapy, specifically in its relationship to brain tumors. To help the understanding of this treatment, I’ll first offer a brief explanation to brain tumors themselves. This central nervous system cancer occurs when the DNA in your cells mutate and a group of brain cells begin to divide uncontrollably. The purpose of T cell therapy is to essentially program your own cells to fight off these mutated, uncontrollable cancer cells in the brain tumor.
T cell therapy, if you are unfamiliar, is an amazing process in which a person’s own immune system (specifically their T cell units) are modified in a laboratory setting to fight off cancer. In other words, T cell therapy is essentially programming a person’s body to do the cancer fighting themselves. In looking up T cell therapy with regards to brain tumors, I came across CAR T-cell therapy which specifically has two types– axicabtagene ciloleucel and tisagenlecleucel. Despite their intimidating names, I came to find that the process of CAR T-cell therapy can be explained quite simply.
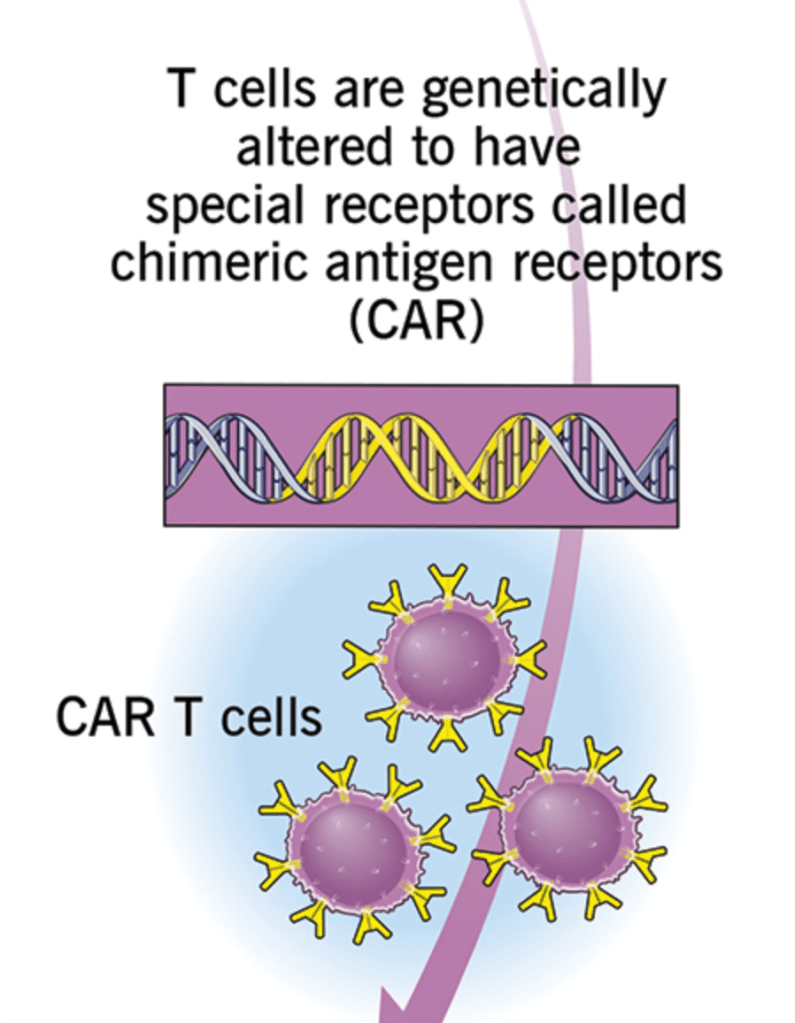
The patient gives a blood sample in which the T cells are removed from the remaining blood cells. Then the T cells receive a specific type of genetic modification (ok, probably not so simple), that gives these cells new receptors called CAR receptors. The patient receives a chemotherapy, and then is presented back with the modified T cells. I was shocked to find that this type of therapy is given in a single treatment. Of course, like all health care in this country, T cell therapy is by no means cheap. The asking price, currently, on this type of therapy is $373,000, with varying reimbursements depending on medicare eligibility. Another con, outside the cost of this therapy, are its side effects. A primarily recognized side effect is the cytokine release that accompanies this therapy, resulting in flu-like symptoms for the patients, usually. Another side effect deals more with neurological function, specifically confusion and impairments speaking. I was personally surprised when reading these side effects, expecting that the implications of re-coding one’s T cells would be far more dangerous and life threatening than the listed side effects appear. After conducting this research, I not only feel more empowered to understand the process of T cells throughout the body, but I also feel compelled to share this data with anyone looking for an answer regarding brain tumor therapy methods.
Extra credit: With regards to COVID-19 cures, it’s undeniable that the world is paused, searching for an answer. Working on what I assume to feel like an emergency time crunch, COVID experts are looking to find fast cures. As a result, a lot of the discoveries that have been made are not empirically proven to work, but are simply guesses. At this point, associations and anecdotal evidence is carrying heavier weight than usual, given the state of such a pandemic. Two drugs being considered specifically are drugs that were used on viruses in the past, specifically on malaria and other diseases that are inflammatory in nature. As of March 24, 2020, only two drugs have offered some type of preliminary result after tireless petri dish testing and manipulation. One drug chloroquine, was studied in China in an experimental setting, and is said to have shown a decrease in pneumonia development in COVID patients.
Another antiviral drug, Remdesivir, has been explored for its potential to have an enzyme that prohibits viruses like COVID 19 from continuing its replication. So far, this drug has shown promising results in the setting of animal testing, facing diseases like SARS that are similar in pathogenesis to COVID 19. Although there is no current cure, there is much to be said behind the closed doors of labs around the world, watching those petri dishes carefully to hopefully bring peace of mind to respiratory systems around the world.
These past few weeks, as the entire world has seemed to come to a dramatic pause, I feel as if I have had to tap deeper into my identity as a student, a senior, a daughter, a sister, and as a friend. Although extremely stressful at times, I have been really trying to take these moments to appreciate as much as I can, and capitalize where it makes sense. In other words, I feel like I have been trying to be as productive and meaningful with my actions during this time and use it as a refocus, while also acknowledging that the stressors of being unemployed and at home make it hard to be as mentally sharp.

For a pass time, I’ve been going on an absurd amount of outdoor walks, making new playlists of music to listen to, and really just trying to stay on top of my school work as much as I can. With my extra energy during the day, I’ve tried to master a Justin Bieber dance on youtube so I can show my friends once we are all free from our quarantine homes (if you’re curious you’ll need to skip to about a minute into the song to see where the dance really picks up).
I’ve really enjoyed the way in which this quarantine highlights the importance of not only having a positive relationship with others, but also yourself. I think this process has presented me (and everyone) with enormous amounts of stress, but having time and space to worth through that and not rush back into daily life is rarely an opportunity given to us. I hope everyone during this time is able to feel a little bit of peace in some capacity!
We all remember that day in 6th grade health class when you knew your gym teacher was not going to be getting into the usual food pyramid shebang. Oh yes, it was time to discuss safe sex. Of course, back in 2013, a lot of things were different. At least at my small North Carolina school, the conversation on the potential repercussions of unprotected sex were limited, because who would be engaging in such an activity? We weren’t married so… no point!
Whether the topic of safe sex is socially acceptable as a conversation piece in your family or school setting, its importance cannot be denied. In this blog, I will offer an educational look into just one commonly transmitted sexually transmitted infections (STI), chlamydia. This STI is bacterial, and therefore transmitted by the passing of bacteria. The bacteria most commonly spreads through sexual activity, whether it be vaginal, anal, or oral sexual contact between two individuals. So ladies, if he said he got it at the gym from a “dirty towel”, stay informed and check him!
This infection stands out to me for a few reasons. The first, that individuals are capable of carrying these infections without actually knowing. Think about the damage capable of spreading from this asymptomatic infection. If you do show symptoms, these are most likely going to be forms of painful urination, vaginal discharge, painful sex, and bleeding between periods for women.
Another reason that makes this STI stand out is its treatment. Although dangerous if left without treatment, this STI can be solved by an antibiotic regimen prescribed by your doctor. All the more reason to go and check it out with a doctor if you’re feeling unsteady about a sexual partner or feeling! Of course, like any antibiotic, the possibility of resistance to this infection is present, and therefore requires doctors and patients to be very careful and intentional with how antibiotics are used to contain the prevalence and incidence of this infection.
The first time I heard about antibiotic resistance I was a semi-unhygenic sixth grader who thought she had just found an excuse to stop sanitizing her hands. I mean, why sanitize if the germs were only learning to get stronger? Of course, a lot has changed in the past nine years, including my understanding of antibiotic resistance, superbugs, and their impact. Within this blog post, I will explain how my sixth grade logic both fundamentally aligns with and dangerously oversimplifies what is now known about microbial resistance.
First I will introduce the concept of a superbug, as I find these to be a very straightforward embodiment of microbial resistance. A superbug is a microbe or germ that has become resistant to the specific type of drug that once killed it. In other words, a superbug can be understood to have adapted to a particular drug, making it ineffective and too weak to kill that microbe. It is also understood that superbugs are more common in places that are actively attempting to kill off germs more frequently, as the larger presence of the antimicrobials allow the particular microbes to learn and adapt against them. This idea, that more attempts to kill the germs actually inspire their adaptation into something stronger, was the foundation of my hygienic rebellion when first learning about germ resistance.
But, as my understanding of microbiology has developed with research on superbugs and resistance, it becomes clear that the angle at which I was understanding resistance was one of a limited and mistargeted nature. The CDC, rather than focusing on resistance to hand sanitizers and soaps, looks to the use of antibiotics as the roots of superbugs. Antibiotic resistance occurs when these antimicrobials kill almost all the intended microbes, while leaving behind the select few that were resistant to the drug. These microbes will then replicate, producing more microbes that like its parent, resistant to the particular antibiotic. The resistant microbes left are those that adapt into the superbugs we fear we will not be able to kill or control.
Antibiotic resistance is not limited to the doctor’s office, as it is also cultivated through US farming practices and procedures. Food producers feed animals antibiotics in order to make them more profitable on the market. So when you see a fatter piece of chicken meat or an extra-shiny apple in the grocery store, you are also seeing the product of antibiotic preservation and enhancement. By consuming these products, you are also consuming the antibiotics that went into their production, consequently introducing the microbes to another antimicrobial against which they could become resistant.
Directly contradicting my original understanding of microbial resistance, the CDC strongly emphasizes the importance of sanitizing hands and food products in order to prevent the spread of superbugs and antibiotic resistance. In other words, misunderstanding resistance like I once did could result in the exact opposite effect that I had intended: the ability of these resistant microbes to proliferate and spread. The impact on the human population can be seen in the form of incurable infections.
As this research has explained, the expanding use of antimicrobials are producing an increase in microbes that are resistant to them. Hopefully this blog post has made clear what was not to me back in the sixth grade: that sanitation practices are not the root of antibiotic and superbug proliferation, but rather effective ways to mediate these adverse effects. Additionally, I hope this blog could communicate the importance of antibiotic consciousness, seeing as increasing one’s exposure to an antibiotic puts them at risk for developing resistance to that antibiotic.

If you knew that the most effective version of a vaccine also had a 1 and 2.4 million chance of becoming virulent, would you opt in or out? This question of balancing the efficacy of the Oral Polio Vaccine with its potential threat is the centerpiece of understanding poliomyelitis–commonly known as polio. As someone who has taken a few courses in statistics, the odds of infection associated with the OPV method seemed extremely promising. In this blog, I’ll provide some background explaining my initial opinion on the two vaccinations, then delve into why this opinion is one that ultimately contributes to the existence of polio around the world.
As stated previously, the allure behind that of OPV is its efficacy. Unlike the IPV, the OPV activates an individual’s immune system, enabling the mucosal layer of the digestive tract to limit the amount that poliomyelitis is replicated within and excreted from the individual. When first conceptualizing this vaccine, its unprecedented capacity to prevent the virulence of polio seemed like a simple choice. But, when reading further into the research discussing poliomyelitis across the world today, I understood what my initial draw towards the OPV preference was lacking. From a perspective emphasizing the vaccine success in one individual, the immune-reacting OPV seemed to be able to put up the best fight. But, when expanding the ultimate goal of the polio vaccine, it becomes evident that the strength of the fight in an individual’s system is less pertinent than the eradication of the disease worldwide.
The World Health Organization differentiates the inactivated polio virus (IPV) from the previously discussed OPV in a few manners. The most significant difference between these vaccine options lies in the very small potential that could come about if adhering to the OPV–the threat of virulence. When weighing this cost from a perspective larger than that of the individual person receiving the vaccine, I believe the need for a switched vaccination becomes obvious. Eradication, by definition, cannot be reached if the 1 out of 2.4 million vaccines is bringing polio about in communities that might not necessarily be affected by it otherwise. Although most of the time extremely effective in preventing polio’s transmission, this vaccine could potentially reintroduce the disease, setting back the push for herd immunity even further. Today, the presence of polio around the world tells the tail of an entity that’s disappearing, but not yet gone. Despite its rarity, the few nations’ that still see polio epidemics exemplify the truth that the small percent of those with the disease still do exist, contracting and transmitting polio to those also at risk. I believe, along with many US policy makers, that the best bet towards establishing herd immunity and eradicating polio, there should be a shift away from the OPV vaccine and towards the inactivated strand that is unable to produce its own virulence.
Prior to this course, my only exposure to the microbiome’s importance came in the form of advertisements. Better “gut health”, according to the media, could promise better skin, metabolism, and weight control– all of which were available in a probiotic package at your neighborhood harris teeter. But, of course, understanding the microbiome extends far beyond the top-selling Kombucha flavors.


One of the oldest, and least glamorous, mechanisms of enhancing microbiome health can be seen in a practice called a fecal microbial transplantation, or a FMT. This technique, with origins tracing back to the fourth century, explored the microbiomes role in pathology in the context of a Clostridium difficile infection. In these cases, the fecal matter of non-infected individuals was used as a way to transfer healthy microbiomes into the infected individuals, showing how healthy microbiomes are a: different than those infected with C. difficile, and b: able to shape the microbiome of the infected individual for the better. Although slightly gross to conceptualize and not for the at-home-solution types, the FMT is a fundamental aspect of understanding the impact of microbiome and disease and should not be ignored by individuals looking for relief from intestinal disease.
If the contents of one’s microbiome are so important for their health and wellbeing, then wouldn’t it be possible to develop a perfect formula for ideal health conditions? Well, from what researchers currently understand about an individuals microbial health is the importance of diversity. In other words, there is no one healthy gut. While the bacteria making up the gut microbe community might differ significantly between individuals, the goal of the microbiome is the same–balance. A balanced microbiome, according to the most recent research, is one that optimizes the immune and metabolic systems of the body. Often called a “superorganism”, the gut bacteria community plays a large role in a human’s immune system, as they control and inhibit the presence of pathogenic bacteria.
Fundamental to understanding the flu and its impact is the role of embracing the unknown. While you might not associate guess-work with vaccine development, the influenza is an unpredictable entity that requires a unique type of problem solving. Due to a phenomena known as antigenic drift, the influenza virus undergoes small changes over time. For the flu viruses themselves, this is great news seeing as these adaptive mutations create a new type of virus that the body’s immune system cannot recognize. And, as these changes continuously accumulate, vaccinations must be created in an anticipatory manner, using past flu strains as a framework to predict the next wave of influenza.
The Center of Disease Control (CDC) suits up every year to understand and hopefully fight the influenza in the best way possible by looking at the infected. These clinical laboratories have spent the flu season, from September to now, looking at the two specific strains of the virus that are having an impact on the population. As of now, the CDC explains that Influenza B has been the most commonly reported influenza virus this year, for both children and adults under the age of 25.
The most significant changes separating this flu season from others is the increase in Influenza B/Victoria virus, one of the two specific subtypes of Influenza B. The CDC also reports that the influenza activity has been in an elevated state for 13 weeks now, with its largest impact on the health of children. To prevent children from having and transmitting the flu, vaccinations for pediatrics have expanded in age availability for this flu season. These new age restrictions offer three different vaccination types for children 6 months or older, 2 years or older, or 4 years or older, allowing younger children to receive different vaccinations to reduce the severity of the flu and the potential to transmit the flu to other ages. Although the efficacy of the flu vaccine cannot be fully evaluated yet, the high rates of infection and the nature of Influenza B can serve as predictive clues into the flus resistance to the vaccine strains. Specifically, looking into the influenza B subtype mutations that have occurred this season could potentially point toward new influenza B strains against which vaccines and our immune systems are not equipped to fight.
A little over twenty years ago, in 1998, a man and his colleagues set out on a research venture that would receive attention and publicity from both health experts and the general public. Andrew Wakefield, head of this research study, conducted an experiment centered around the relationship between the MMRV vaccine and a child’s development of autism. More specifically, as laid out in an article found at the National Center of Biotechnology Information, this study suggested that this particular vaccine could serve as a predisposition for a child to develop “pervasive developmental disorder”.
This study has since been retracted for many reasons, one of which is due to the extremely small sample size selected by Wakefield. In this study, Wakefield only had 12 child participants. This low number of participants limits the ability of this study to be generalized to any group outside of the one chosen by Wakefield and his 12 colleagues. A larger criticism on the nature of this study was its intent, as it became known that Wakefield and his selected colleagues were specifically paid by a lawyer to find an association between vaccines and autism. This type of bribery, as explained in the British Journal of Medicine, comprises the information produced by the study as it was manipulated with the intent of personal gain for Wakefield and those he self-selected to be in his study. With intent to profit off of a lawyer who had been involved with lawsuits between parents and vaccination companies, Wakefield self-selected a cohort that would support this biased and motivated scientific approach to the research.
Researchers responded to Wakefield’s study by doing what they do best, more research. Seventeen years after the publishing of Wakefield’s original controversial study, produced the largest research study to date looking further into this relationship. With a much larger sample size, this time 95,000 children across the US, the researchers confidently concluded that there was no association between the MMVR vaccine and autism. This response by scientists and those passionate about the integrity of honest research displays the attempt to reconcile any unwarranted controversy and quell unwarranted anti-vaccination sentiments that may have resulted from Wakefield’s study.